Today ACT UP Dublin held a demonstration outside the HPRA offices in Dublin to demand action from the Government and HSE to make PrEP available in Ireland without further delay. Our press release is available for download here.
This is the full text of the press release:
FOR IMMEDIATE RELEASE
August 4, 2017 2:00pm
Contact: act.up.dublin@gmail.com
www.actupdublin.com
PrEP STOPS HIV: Ireland needs PrEP now.
ACT UP Dublin today called on the Irish Government to make PrEP (Pre-Exposure Prophylaxis) available through the HSE immediately.
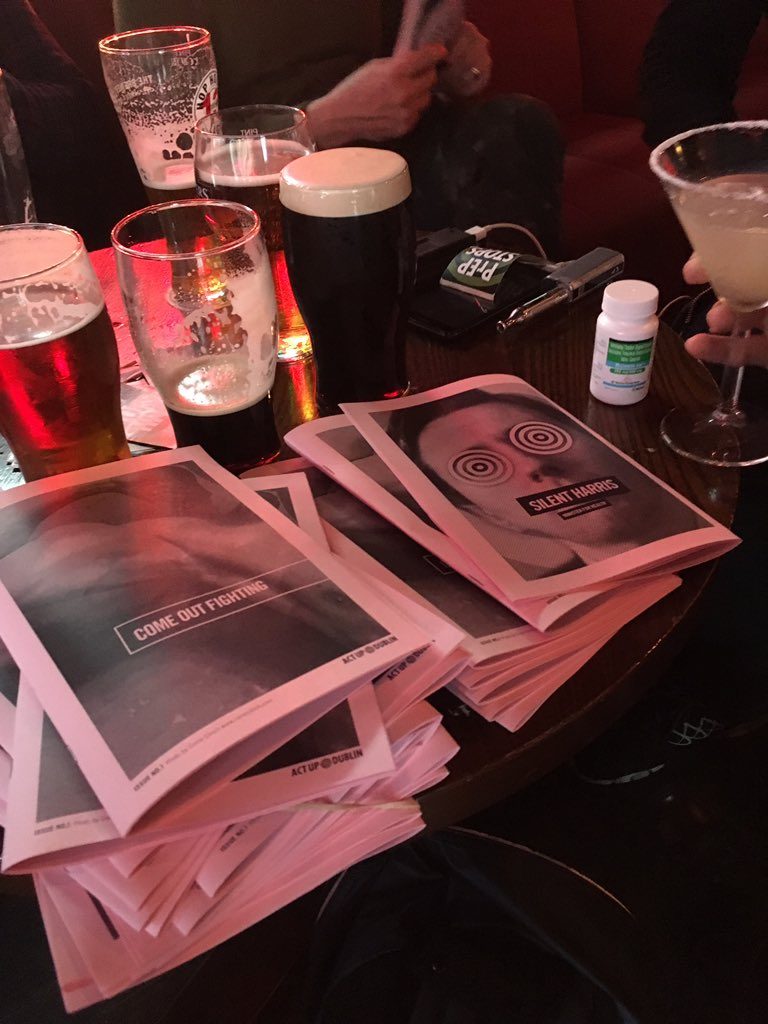
Angered by recent reports of increased seizures of generic PrEP by Irish Customs, and the HSE’s failure to provide even limited access through a pilot PrEP programme, advocates gathered in front of the HPRA offices on Earlsfort Terrace at lunch time to demand that the Minister for Health, Simon Harris, make a commitment to address Ireland’s HIV crisis and make PrEP available and accessible in Ireland without further delay.
New HIV diagnoses in Ireland are at record levels with one new HIV diagnosis every 18 hours. Delays on PrEP lead directly to entirely avoidable new HIV infections.
We know more about HIV treatment and prevention than ever before…
yet new diagnoses continue to rise.
Powerful new tools like PrEP have the potential to dramatically impact the epidemic…
yet they are unavailable here.
It’s time for this Government to show that it’s serious about Ireland’s HIV crisis.
It’s time for leadership instead of foot dragging.
It’s time for PrEP in Ireland.
————————
In 2015, Ireland reported the highest number of new HIV diagnoses in the history of the epidemic. Preliminary figures from 2016 are even higher. The LGBT community has been particularly impacted as new HIV diagnoses among gay and bisexual men quadrupled between 2005 and 2015.
Pre-Exposure Prophylaxis for HIV—better known as PrEP—is a safe and highly effective way for HIV-negative people to prevent HIV using antiretroviral medication. The World Health Organization recommends that PrEP be offered to people at substantial risk of HIV as part of a comprehensive HIV prevention package.
Currently only one medication, Truvada, has been approved for use as PrEP in Europe. Although doctors in Ireland can prescribe Truvada as PrEP, the HSE does not yet provide reimbursement for the medication. Purchased privately through a pharmacy in Ireland, Truvada would cost hundreds of Euro per month—much more than anyone can realistically afford.
A growing number of people in Ireland, fed up with the Government’s failure to provide access to PrEP, are taking responsibility for their own and the community’s health. Following a model established in the UK (where it is legal to import generic medication for personal use) they are purchasing generic versions of PrEP online. In the UK, the widespread use of these generics is credited with helping to produce a dramatic reduction in new HIV diagnoses among gay and bisexual men in the last year.
UK-based websites like iwantprepnow.co.uk provide comprehensive information about PrEP—how it works, how to use it, how to get the necessary clinical support—and provide links to sites known to be reliable sources for authentic generics.
Unfortunately, the HSE currently provides no formal, dedicated clinical support services for PrEP users. Although the tests can be obtained through existing health services, those who are able to source more affordable generic versions online must manage their own clinical care. There is no consistent clinical monitoring by properly-trained medical providers, no systematic data about current PrEP users is being collected, no official information is available for current or potential PrEP users.
Instead of making PrEP available directly, or offering badly needed clinical support services to those who are taking initiative and already using PrEP, Irish health authorities are seizing packages, harassing suppliers, and trying to undermine public confidence in the only available route to obtaining PrEP for people in Ireland.
It’s time for Minister of Health, Simon Harris, to show leadership in tackling Ireland’s HIV crisis.
Making PrEP available in Ireland without further delay must be a priority of this Government.
What is ACT UP?
ACT UP Dublin is a local chapter of ACT UP, The AIDS Coalition to Unleash Power, an international HIV activist organisation. ACT UP Dublin was founded in July 2016 to take action on Ireland’s HIV crisis. We seek a more urgent and effective response to HIV from government, community organisations, and the public at large.